At Axial HealthCare we are committed to provide accurate, timely and effective billing and credentialing service. Our highly trained medical billing staff is an extension of your office. We employee experts and keep up with the latest technologies to provide you best in the industry.

Provider credentialing is the process of getting a physician or a provider affiliated with payers is a critical step in the revenue cycle. The process enables patients to utilize their insurance cards to pay for medical services consumed and enables the provider to get reimbursed for the medical services provided. Axial Healthcare understands the necessary process of credentialing and health insurance enrollment required of healthcare providers when running a practice or setting up a new practice. As a participating provider in the insurance company's preferred network, you will have the opportunity to grow your practice and expand your patient base. But as important as the health insurance enrollment and credentialing process are, they are also time-consuming, redundant, and can take a long time to finish, especially if any mistakes are made along the way. Medicare provider enrollment is particularly complex when it comes to knowing the correct form(s) to submit or whether to use PECOS for an on-line application. And what is CAQH? Is that needed too? Axial Healthcare assists healthcare providers of all specialties in the payer enrollment process with government and commercial payers. We coordinate with insurance companies to initiate and maintain accurate credentialing statuses. Axial Healthcare ensures that the process of getting providers credentialed with new payers or plans in timely and has clean claim submissions. We negotiate contracts on your behalf. Our credentialing services are handled by an expert team with 15+ years of experience.

Axial Healthcare has a scrupulous team of both AAPC (American Academy of Professional Coders) & AHIMA (American Health Information Management Association) certified specialty-specific coders & auditors who strictly adhere to US Healthcare Insurance & Federal regulations. We continuously impart professional training in medical coding to all our coders to ensure that they remain well informed and updated with the latest developments. Our in-house medical coding services team are highly experienced with extensive coding domain knowledge and precise analyzing skills. We aim to improve hospital and physician profiling and scorecard data to position hospital for growth and improve external reputation without compromising on quality.
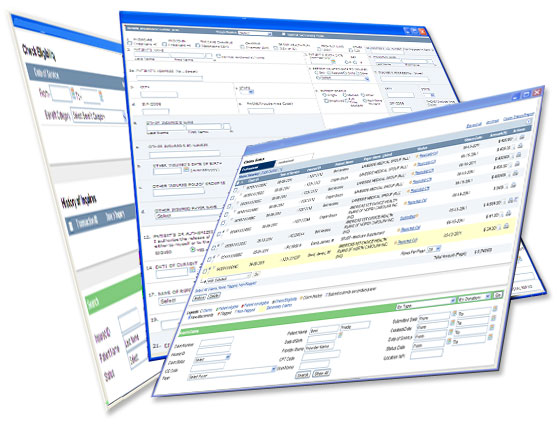
Hospitals and healthcare facilities face a lot of hassles when it comes to settling payments with regards to insurance. Payments are considered settled when patients submit insurance details at the front desk of the hospital. But the hospital or healthcare facility does not receive the final payment until the insurance agency settles the claim. Our medical billing services allow hospitals to take the back-seat through the various steps involved in the process. To simplify the medical billing process and minimize the daily hassles encountered by hospitals and other healthcare facilities, Axial Healthcare follows best in industry Six Sigma techniques and with an expert team of 15+years' experience as Billing managers, Axial Healthcare is the right choice for your healthcare business.

Healthcare Providers and medical billing companies lose a lot of money due to a lack of follow-up on outstanding claims with the insurance companies. Axial Healthcare has a dedicated AR follow-up team that aggressively follows-up with insurance companies on all accounts. Our AR management team is structured to be a complete solution for the provider to address difficulties that occur in cash flows and is operated as a part of the medical billing team. Our team constantly keeps in touch with insurance companies via websites, fax, IVR, and phone to ensure that claims are settled quickly. We aim at accelerating cash flows and reducing the Accounts Receivable days by submitting error-free clean-claims, proper analysis of denied claims and regular follow-ups with insurance companies and patients for outstanding claims and dues. The AR management team continuously monitors the aging buckets of the ARs and guarantees that all the claims are followed upon between 25-45 days from the date of entry depending on the payer. Axial Healthcare's goal is to recover the funds owed to the client as quickly as possible.

Many a time, practices and Facilities have accumulated unresolved Accounts Receivables either through lack of proper AR follow-up due to lack of manpower or sometimes they end up with these backlogs due to poor AR Management done by another medical billing company. Axial Healthcare team analyzes the various accounts receivable reports provided by the client and determine strategies to work on the AR management strategy. The strategies are developed and executed, so that there is a reduction of the bad debts and AR collections are maximized. Also we have a dedicated patient calling team where we offer the services like,